
Have you felt energized/high/out of control lately?Īnxiety, depression, schizophrenia, dementia, delirium, substance abuse Have you felt angry/irritable/on edge lately? Have you felt discouraged/low/blue lately? Mood: patient's subjective report of emotional stateĭepression, bipolar disorder, anxiety, schizophrenia Volume and tone: loud, soft, monotone, weak, strong, mumbledįluency and rhythm: slurred, clear, hesitant, aphasicĪffect: physician's objective observation of patient's expressed emotional state Schizophrenia substance abuse depression bipolar disorder anxiety medical conditions affecting speech, such as cerebrovascular accident, Bell palsy, poorly fitting dentures, laryngeal disorders, multiple sclerosis, amyotrophic lateral sclerosis Quantity: talkative, expansive, paucity, poverty (alogia) Tendency toward exaggerated movements occurs in the manic phase of bipolar disorder and with anxiety Symptoms may develop within weeks of starting or increasing dosages of antipsychotic agentsĬatatonia: neurologic condition leading to psychomotor retardation immobility with muscular rigidity or inflexibility may present in excited forms, including excessive motor activity

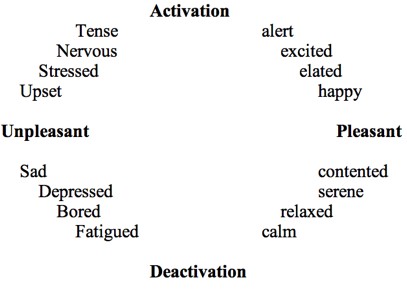
Parkinsonism, schizophrenia, severe major depressive disorder, posttraumatic stress disorder, anxiety, medication effect (e.g., depression), drug overdose or withdrawal, anxietyĪkathisia (restlessness), psychomotor agitation: excessive motor activity may include pacing, wringing of hands, inability to sit stillīradykinesia, psychomotor retardation: generalized slowing of physical and emotional reactions Irritability may occur in patients with anxietyīody posture and movement, facial expressions Paranoid, psychotic patients may be guarded General behavior: congenial, cooperative, open, candid, engaging, relaxed, withdrawn, guarded, hostile, irritable, resistant, shy, defensive Poor eye contact may occur with psychotic disorders Unkempt appearance may suggest depression, psychosisĮye contact: good, fleeting, sporadic, avoided, none Provocative dress may suggest bipolar disorderĪppearance: well-groomed, immaculate, attention to detail, unkempt, distinguishing features (e.g., scars, tattoos), ill- or well-appearing The mental status examination can help distinguish between mood disorders, thought disorders, and cognitive impairment, and it can guide appropriate diagnostic testing and referral to a psychiatrist or other mental health professional.īody habitus, grooming habits, interpersonal style, degree of eye contact, how the patient looks compared with his or her ageĭisheveled appearance may suggest schizophrenia In such situations, specific questions and methods to assess the patient's appearance and general behavior, motor activity, speech, mood and affect, thought process, thought content, perceptual disturbances, sensorium and cognition, insight, and judgment serve to identify features of various psychiatric illnesses. A mental status examination may be beneficial when the physician senses that something is “not quite right” with a patient.
Major challenges include incorporating key components of the mental status examination into a routine office visit and determining when a more detailed examination or referral is necessary. The mental status examination includes historic report from the patient and observational data gathered by the physician throughout the patient encounter. Familiarity with the components of the examination can help physicians evaluate for and differentiate psychiatric disorders. The mental status examination is an essential tool that aids physicians in making psychiatric diagnoses.


 0 kommentar(er)
0 kommentar(er)
